
For people with moderate to severe psoriasis, the treatments based on highly targeted antibodies that have been provided in the past ten to 15 have changed life. The inflamed skin that completely covers the areas of the body is completely solved. “It is difficult to find a respondent for these treatments,” says Cordin Konrad, clinical dermatologist and psoriasis researcher at Lausanne University Hospital in Switzerland.
Nature expectations: skin
But these antibody treatments, which selectively take the inflammatory molecules that lead the disease, have a major defect: they should be taken for life. If the treatment stops, the disease is back.
At least, this is usually happening. Some people with psoriasis can stop taking antibodies and have no relapse. Konrad says that one of his patients who were taking antibody drugs had to stop him in preparation for the dental process-and that “after six years, she was still completely free of diseases, not a single lesion.”
When large clinical trials test this phenomenon, and increase researchers from detecting the basic molecular mechanisms of psoriasis, excitement increases that new treatments for this disease may be more durable.
Chemistry is a biochemistry
Psoriasis affects at least 100 million people all over the world, and is currently not a treatment1. More visible symptoms of this unknown disease is the presence of inflamed painful skin lesions, called paintings, which are colonized by excessive immune cells. However, the inflammatory damage to the psoriasis deepens. People with psoriasis are at risk of developing cardiovascular disease, diabetes and arthritis. The quality of life and weak stigma can affect mental health.
Australia, Australia, who is studying this first stage of the disease, says the vital molecular trigger that begins the excessive activation of immune cells in the affected skin is still a mystery. “It is difficult to pick up that moment at the beginning, so we still don’t know what starts with it,” she says. But by comparing psoriasis and healthy skin, a clear image of the chain of inflammatory signal particles, or cytokines, which lead the condition. Return, Brown says, “We now know how to control the cytokines series.”
Antibody treatments target one of the three main cytokines: tumor necrosis factor (TNF-α); Intercin 17 (IL-17); Or Interleukin 23 (IL-23). Preventing any of these closes inflammation in the affected skin. The leading treatments in the Novartis SECUKINUMAB in Basel, Switzerland, targeting IL-17, and Guselkumab from Johnson & Johnson in New Bronzwek, New Jersey, targeting IL-23.
On the trial
Although antibody treatments are safe and effective, taking rates for lifelong system are fears. Lev Edsmo, a doctor and psoriasis researcher at the Carolinska Institute in Stockholm, says the long -term use of these drugs “systematically changes a person’s immune balance.” For example, a TNF-α ban can increase the risk of non-metacular skin tumors, and an IL-17 ban can lead to inflammatory bowel disease. “However, we cannot stop treatment, so we are stuck,” says Edsmo.
To find a way out of this trap, researchers study 10-20 % of people with psoriasis whose condition is not transferred for several months or even years after stopping treatment. In one of the experiments, the researchers gave individuals with moderate psoriasis to severe SECUKINUMAB for one year, then stop treatment and monitor how quickly their condition is settled.2. The main factor was at the time of relapse, after the time after the appearance of the disease that started treatment. “Patients suffering from a short disease, they started treatment within a year from the beginning, they have been relaxing for a long time,” says Conrad. In those who waited for a longer time to start treatment, the remaining possibilities were gradually free of relapse. People who suffer from the history of the disease for five years or more before starting treatment have quick relapses.

LIV EIDSM is a psoriasis researcher at the Carolinska Institute in Stockholm.Credit: Carolinska Institute
If a treatment for antibodies is given early enough, the results indicate that lifetime treatment can be avoided. “We now know that we have a window of opportunities to adjust the disease, as we can treat the patient to enter a remission – then it is possible that he will open them out of treatment completely,” says Conrad.
Konrad and Eidsmo participate in the first psoriasis experience designed for an early intervention test, followed by treatment withdrawal. Stepin’s study tracked one -year later of the SECUKINUMAB treatment in people who became a severe psoriasis within 12 months of its development.
By the end of the first year, more than 90 % of people who treated a 90 % decrease or more have witnessed the severity and spread of their disease3. Then the treatment was withdrawn. The results in the second year are expected to be known before the end of this year. If a large number of people remain free of diseases, it may have great repercussions when giving this treatment. “If early treatment leads to a smaller disease, it may be the way to go,” says Eidsmo.
Meanwhile, the trial of evidence in pointed doses is achieved after early interference with Guselkumab antibodies. Konrad says: After that in IL-23 it looks more effective than targeting IL17, perhaps because it is higher than the chain of psoriasis. The results of the initial evidence showed that the participants who completely cleared their skin after early intervention can be the frequency of doses in half4. The final stage of the guide will test the cessation of full treatment.
Clinical effect
Early intervention experiments have already changed the treatment of psoriasis in the clinic. “For patients who become very severe, we can give them early access to these medications,” says Conrad. Early intervention is likely to convert their exhausted disease into a mild that can be controlled with topical treatments from time to time.
Although clinical trials have focused on moderate to severe psoriasis, people with mild disease – the most common form – can also benefit from early intervention. In a study conducted in 2022 led by John Fur, a dermatologist at New South Wales University in Sydney, Australia, the researchers gave an early treatment for antibodies to people with psoriasis in Guttate5. This moderate form of psoriasis is usually solved quickly, but 30 % of people apply to chronic psoriasis. “Our study showed that you can intervene early and reduce the risk of this progress.”
The mechanism with early intervention reduces the risk of relapse is still unclear. The initial focus has decreased on T -cells, a type of immune cell that has long been linked to psoriasis. Usually, the Ti -cells patrol in the body for the specific peptides produced by pathogens. In psoriasis, some T-cells accidentally begin to respond to the body’s peptides-the trigger that has not been determined after that Brown is looking for.
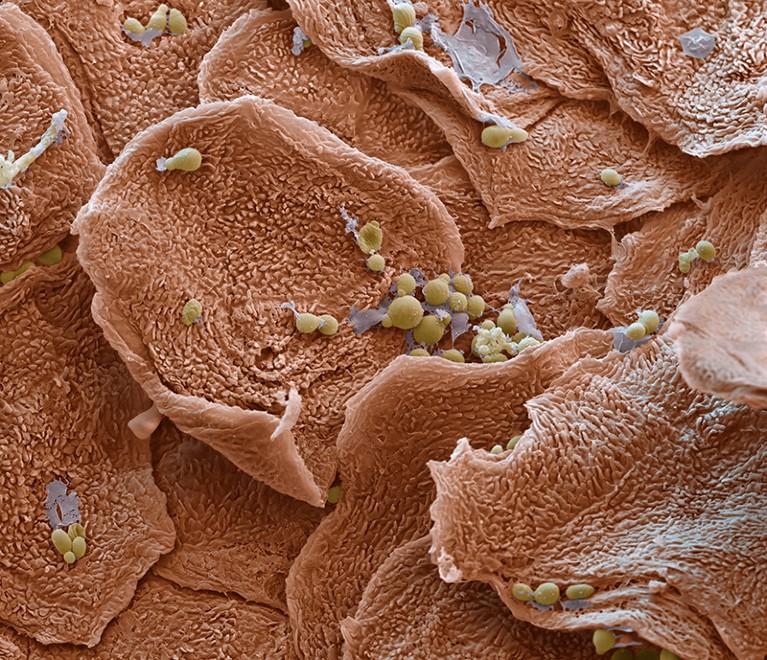
Poles of dry, exfoliated skin that are colonized by excessive immune cells are symptoms of psoriasis.Credit: Science Photo/Science Library
A type of T -cell known as the residing memory in the tissue (tRM) Cell is permanently concentrated in the skin, and is increasingly identified as a major psoriasis player. In the clinical trials of antibody treatments, “you always see a decrease in this TRM“The cells, when the treatment stops, the levels of R.RM The cells rise again in people whose disease relaxes, and the return of skin plaques. R.RM Thus, the cells are the goal of the clear psoriasis. But there is a discussion about whether to eliminate them is a good idea because Conrad, “the vast majority of R.RM [cells] In the skin it protects us from pathogens. “
Instead of exterminating R.RM Cells, Braun hopes that you can rehabilitate cells by identifying the peptides that disturb R.RM Cells are the wrong definition as a threat. “Once we know the trigger peptides, we can develop a reverse vaccination that revives the immune system that this peptide can be ignored safely,” she explained.
Eidsmo also targets RRM Cells, focusing on many people who suffer from psoriasis who never progress from moderate diseases and who has improved treatment options since the 1990s. “I would like to know how to treat T locallyRM Cells in moderate cases.
Treatment
T treatmentRM Conrad says the cells are not the only possible way to forgive the psoriasis. Instead of T -cells – part of the adaptive immune system – Conrad focuses on fungal immunity, an ancient form more evolutionary than defense.
For decades, the general understanding of innate immunity was that unlike adaptive immunity, it was not possible to learn from the confrontations of previous nurses. But over the past fifteen years, this idea has turned. Scientists now know that once the innate immune system fights one invaders, it can fight more effectively.
This fungal immune memory has direct effects on psoriasis. In 2017, researchers who study psoriasis in mice showed that immune memory in the skin cells is called keratin cells that were driving the condition6. The team showed that the immune memory of the keratini cells was based on the reprogramming of the Lagini-molecular illustrations to its DNA, which put a reference signal on the genes of stress, and the settlement of its chronic inflammatory behavior.
More nature expectations
Lagine immune memory plays a major role in psoriasis. Frew says: “We know now, that fungal ingredients remain present even after a clinical remission of psoriasis” after treating antibodies. “Although you may be completely clear about clinical diseases, there are still some remaining inflammatory scar.”
Konrad says that this gradual accumulation of Lajini delegation is what explains the early treatment window to adjust the pathological cycle. “The intervention with the treatment of antibodies early may be the prevention of such Lagin changes, or their opposite,” he says.
Evidence points in this direction as well. In a genetic analysis presented at the Dermatology Conference in 2023, the participants participated in the Stepin Early-invention experience who had the disease for less than a year when treatment began in the Lagini-shaped in the form of analogous DNA reflected to normal levels after 12 months. On the contrary, people who have been ill for more than five years have more clear genetic scars before treatment, and they are still suffering from remaining scars a year after the treatment of antibodies.7.
Perhaps, with longer treatment, this scarring may fade in the end. “The next question is, can we add something alongside the treatment of antibodies that directly affect Lagino change?” Conrad says. If a second treatment can erase these lagin reference signals, it may be possible to stop the treatment of antibodies without leading to lighting psoriasis.
With multiple lines of research targeting T cells and fungal immune memory, the next decade can transform psoriasis, says Conrad. “Ten years ago, I thought we would not treat psoriasis in my life,” he says. “Now, I think we will be able to treat some patients during the contract.”
