Fergus WalshMedical editor
A group of blind patients can read again after being fitted with a life-changing implant at the back of their eye.
The results of the international trial are “amazing”, says the surgeon who inserted microchips into five patients at Moorfields Eye Hospital in London.
Sheila Irvine, 70, who is registered blind, told the BBC it was “out of this world” to be able to read and do crossword puzzles again. “It’s beautiful and wonderful. It gives me such pleasure.”
This technology offers hope for people with an advanced form of dry age-related macular degeneration (AMD), called geographic atrophy (GA), which affects more than 250,000 people in the UK and five million worldwide.
In people with this condition — which is more common in older adults — cells in a small area of the retina at the back of the eye gradually become damaged and die, leading to blurred or distorted central vision. Fine colors and details are often lost.
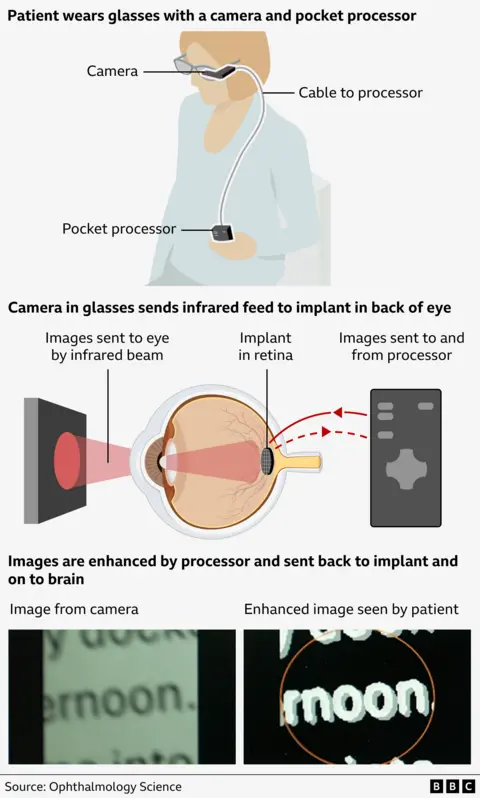
The new procedure involves inserting a tiny photoelectric chip measuring 2 square millimeters, the thickness of a human hair, under the retina.
Patients then wear glasses that have a built-in video camera. The camera sends a beam of infrared video images to the implant at the back of the eye, which sends them to a small pocket processor to enhance them and make them clearer.
The images are then sent back to the patient’s brain, via the implant and optic nerve, giving them some vision again.
Patients spent months learning how to interpret the images.
Mahi Moukit, a consultant eye surgeon at Moorfields Eye Hospital in London, who led the British part of the trial, told the BBC that it was a “pioneering, life-changing technology.”
“This is the first implant that has been proven to give patients meaningful vision that they can use in their daily lives, such as reading and writing.
“I think this is great progress,” he said.
How does the implant technique work?
For research published in New England Journal of MedicineThirty-eight patients with geographic atrophy in five European countries participated in a trial of the PRIMA implant, made by California Biotech Sciences.
Of the 32 patients given the implant, 27 were able to read again using their central vision. After a year, this was equivalent to an improvement of 25 letters, or five lines, in the eye chart.
For Sheila, from Wiltshire, the improvement is even more dramatic. Without the implant, she is completely unable to read.
But when we filmed Sheila reading an eye chart at Moorfields Hospital, she didn’t do anything wrong. After she finished, she punched the air and cheered.
“I’m a happy bunny”

The task took great focus. Sheila had to place a pillow under her chin in order to stabilize the feed from the camera, which could focus on only one or two letters at a time. At some points, she needed to turn the device to zoom mode, especially to distinguish between the letters C and O.
Sheila began losing her central vision over 30 years ago, due to the loss of cells in the retina. She describes her vision as being like having two black discs in each eye.
Sheila gets around with a white cane because her very limited peripheral vision is completely blurred. She is unable to read even the largest street signs when outside.
She says she cried when she had to give up her driver’s license.
But after having the implant fitted about three years ago, she is happy with her progress, as are the medical team at Moorfields.
“I was able to read my posts and books, do crossword puzzles and do Sudoku,” she says.
When asked if she thought she would ever read again, Sheila replied: “Not on Nelly!”
“It’s amazing. I’m a happy bunny,” she adds.
“Technology is moving so fast, it’s amazing that I’m a part of it.”

Sheila does not wear the device when outside. This is partly because reading requires great concentration, as her head must remain very still in order for her to read. She also doesn’t want to be overly dependent on the device.
Instead, she says she “rushes through her chores” at home every day before sitting down and putting on her glasses.
The Prima implant has not yet been licensed, so it is not available outside of clinical trials, and it is not clear how much it might ultimately cost.
However, Mahi Moqit said he hoped it would be available to some NHS patients “within a few years”.
This technology could be used to help people with other eye diseases in the future.
Dr Peter Bloomfield, director of research at the Macular Society, says the results are “encouraging” and “great news” for those who currently have no treatment options.
“Prosthetic vision may offer a lot of hope for many, especially after previous disappointments in the world of dry AMD treatment.
“We are now watching closely to see whether the Prima implant will be approved for use here in the UK and, more importantly, whether it can be made available in the NHS.”
A transplant will not help restore sight in people born blind, because they do not have a functioning optic nerve to pass signals to the brain.