
Jim Reed,Health correspondent,
Wesley Stevenson,Verified by BBCand
Nick Triggle,Health correspondent
 Getty Images
Getty ImagesHealth officials say the NHS remains on high alert over flu, but there are clear signs that the virus surge has come to an end at least for now.
The UK’s Health Security Agency says community spread appears to have stabilized.
Meanwhile, the rise in hospitalizations has slowed. With just over 3,000 patients in hospital in England with the virus, NHS chief executive Sir Jim MacKay’s dire prediction of “between 5,000 and 8,000” cases has not come true.
How severe has this flu season been so far, and how does it actually compare to previous outbreaks?
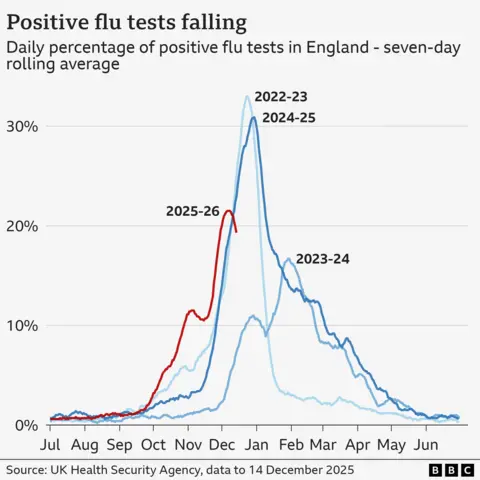
The main difference between the 2025 flu season and the past three years is that the virus began spreading a few weeks earlier than normal.
When someone goes to their GP or hospital with flu-like symptoms, they can be swabbed and tested for flu, Covid, RSV and other viruses.
The UKHSA then records the percentage of those tests that come back positive for influenza.
The numbers rose rapidly during the fall and early winter.
But the spread of the virus appears to have stabilized last week at a moderate level, the UKHSA says.
It is too early to say whether this marks the beginning of the peak. Flu is unpredictable, and a lull can be followed by another wave.
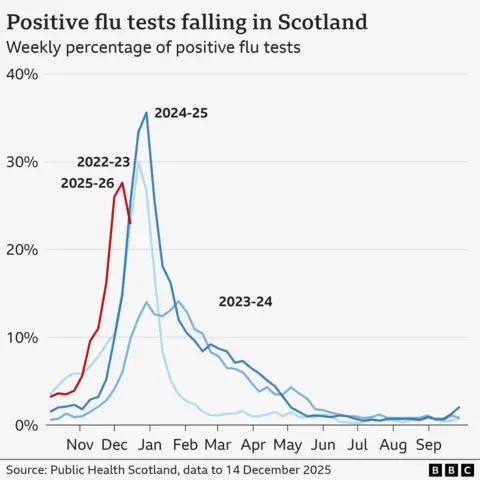
The picture in the four UK nations is similar.
Some virologists linked the previous flu season this year to the circulating virus type known as H3N2.
Historically, seasons dominated by this strain tend to be more severe, with higher numbers of hospitalizations in the elderly, in particular.
H3N2 has not been the main form of influenza detected in the UK for three years, which could mean less immunity has been built up in the population.
Scientists also detected an additional shift in the genetic makeup of the virus over the summer.
This appears to have given the virus a head start in the fall.
Can we call it the super flu?
The name ‘super influenza’ has been used by the NHS to describe this latest outbreak.
But that’s not a medical term, and it doesn’t mean that the virus itself has suddenly become more dangerous or harder to treat.
“It’s a bit misleading and scary to call it a superflu; it’s just a type of flu that’s obviously a little more contagious than usual,” says Professor Lawrence Young, Professor of Molecular Oncology at the University of Warwick.
“What we are seeing is a flu season that may be two to three weeks earlier than usual.”
Separately, the NHS also records the sickest patients in hospital with flu during the winter. Trends in hospital data tend to lag behind community spread, as it takes time for people to get sick enough to require hospital care.
Last week’s figures showed that the number reached 3,140, an increase of 18% from the previous week. But that was after a 55% jump the week before that.
Although the national figure masks what is happening in different regions, with some regions seeing a decline in numbers and still others seeing a sharp rise.
People over the age of 85 are five times more likely to be hospitalized than the general population.
It’s difficult to compare outbreaks over past decades because testing has improved in recent years, so a rise in hospitalizations over time may also reflect better detection.
But estimated numbers of deaths from influenza show that some winters have been particularly dangerous over the past 20 years.
In 2017-18, for example, 25,000 people are thought to have died from the virus in England, with care homes and elderly people hardest hit.
That year, an unusual form of influenza B virus began to spread, and the “Beast from the East” cold snap brought freezing temperatures to the UK, creating the perfect environment for the disease to spread.
Just three years earlier, in 2014-15, modeling by scientists at the UKHSA estimated that 35,000 people had died, making it one of the deadliest flu seasons in decades.
Again, this was blamed on the H3N2 outbreak and the seasonal vaccine that did not match well the exact form of the disease circulating.
There’s nothing in the data yet to suggest anything comparable to 2025, but we won’t know for sure until the first estimates of flu deaths this season are published in the new year.
The message from doctors and the NHS is for millions of people to continue to come forward to get the flu vaccine.
Although the genetic makeup of the virus has changed, the main vaccine is still thought to provide an effective level of protection, particularly against ending up in hospital with severe illness.
The flu vaccine is free on the NHS for over-65s, young children, pregnant women, people with certain health conditions, carers and frontline health and social care workers.
All other adults can get the same vaccine for between £15 and £25 from high street pharmacists.
More than 70% of older people and care home residents had taken up the offer of a free vaccination by 14 December, the latest data shows.
But vaccination rates in some other groups are much lower.
Only 45% of all NHS frontline workers in England have been vaccinated so far this year.

