
Michael Levine had just started working as a pediatric infectious diseases doctor in London when he received an urgent call from a hospital in Malta. It was the early 1980s, and a young boy was brought to the hospital with symptoms of a severe infection that was spreading through his body, damaging multiple organs and tissues. But his doctors could not find any trace of pathogens.
The specter of influenza past and the search for a universal vaccine
The boy was airlifted to Levin Hospital for further testing. To the surprise of Levin and his colleagues, the culprit was a common bacteria: Mycobacterium fortuitumwhich live in water and soil, and are usually harmless. “Everyone is exposed to it, but almost no one gets sick,” says Levin, who now works at Imperial College London. Despite aggressive treatment, the boy eventually died.
This case illustrates a question that has plagued doctors for decades: Why do some people become so ill from infections that leave others unharmed? What makes some people’s immune systems vulnerable to infection? How might these differences affect how doctors try to prevent or treat disease?
As it turned out, the boy from Malta had a brother and a cousin who also became severely ill with mycobacterial infections. After years of research, Levin and his colleagues eventually identified what made these children so sick: a genetic mutation that affects the interferon-γ receptor, an immune molecule with countless functions, including regulating inflammation.1. Shortly after that, a team in France discovered that similar mutations were responsible for rare cases of severe disease caused by another type of fungus — this time, a weakened form used as a tuberculosis vaccine.2.
Researchers have since assembled an extensive library of mutations in hundreds of genes that underlie the “innate immune errors” (IEIs) that leave millions of people around the world vulnerable to a wide range of infectious and immune-related diseases that many people can simply ignore.
It may seem obvious that differences in each person’s immune system can affect how well they are able to resist pathogens. But uncovering the specific reasons for this difference has enabled researchers to find ways to treat — and even prevent — severe infections that once seemed like random cases of bad luck, says Isabelle Metz, an oncologist and immunologist who studies IEIs at KU Leuven in Belgium.
These discoveries are already beginning to change clinical practice, for example allowing doctors to genetically screen people for relevant mutations or supplement missing immune factors. Scientists continue to piece together the many ways in which genetic factors contribute to infectious diseases, especially in life-threatening cases. “What we are realizing more and more is that there are likely inherited factors that predict who will have severe reactions,” says Michael Abers, a physician and scientist who studies infectious diseases at Montefiore Einstein Hospital in New York City.
From microbe to host
The germ theory of disease, popularized by Louis Pasteur in the 19th century, was revolutionary. The realization that microorganisms, invisible to the naked eye, can make people sick has spurred public health measures such as improved hygiene, vaccines, and antimicrobial drugs, which have dramatically improved outcomes for people with infectious diseases.
But even with the use of these tools, there are still people — especially some children and the elderly — who get sick and die from diseases that are usually preventable or treatable, suggesting limitations in focusing mostly on pathogens in the fight against infectious diseases.
In the 1950s, some scientists had already drawn attention to the importance of the host, especially in cases where harmless microbes cause disease. Researchers have since discovered that one of the most important factors determining susceptibility to infection may be a person’s genes.
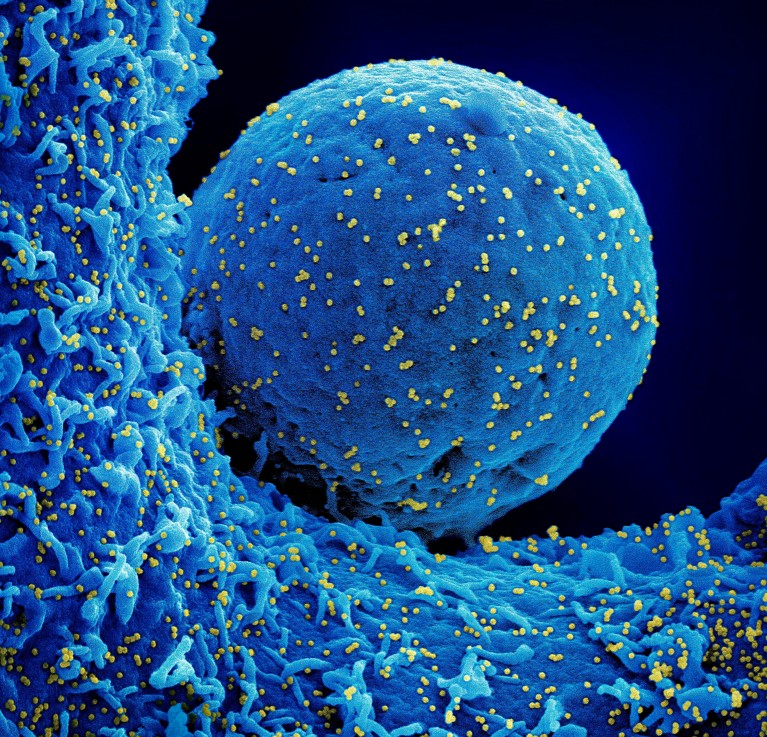
SARS-CoV-2 virus particles (yellow) infect the cell (blue).Credit: NIAID/NIH/SPL
Among the best-known evidence of genetic mutations driving infection outcomes is severe combined immunodeficiency (SCID), a genetic disease that leaves people without a functioning immune system and is associated with mutations in more than a dozen genes. If left untreated, it usually leads to death before the age of two.
Fortunately, SCID is rare, occurring in an estimated 1 in 50,000 births or so. But inherited mutations that can cause problems with the immune system are more common. Over the past few decades, researchers have discovered inborn errors in immunity linked to more than 500 genes3. In addition to susceptibility to infectious diseases, these mutations are involved in other abnormalities of the immune system, including autoimmune diseases and allergies.
Some mutations weaken the immune system and reduce its ability to fight infection. But others can cause people to overreact to infections, potentially leading to runaway immune reactions that can become fatal.
Although some IEIs can cause a general vulnerability to pathogens, most put people at risk of infection with specific microbes, such as mycobacteria, avian influenza virus, herpes simplex virus, and bacteria. Neisseria meningitis.
“Every infection has a different set of mechanisms,” says Steven Holland, a physician and infectious disease scientist at the National Institutes of Health (NIH) in Bethesda, Maryland. “Unsurprisingly, there are different genes that deal with” different types of infections. The mutations known so far tend to cause severe disease, although some are associated with milder recurrent infections.
Furthermore, there are genes that can enhance a person’s ability to fend off pathogens. For example, a mutation in the gene encoding CCR5, a receptor found on the surface of white blood cells, makes people resistant to HIV.4 (Although it increases the risk of severe West Nile virus infection.) Mutations in the gene that encodes FUT2, a protein found in the intestinal mucosa, help people ward off norovirus, a highly contagious gastrointestinal infection.
Expanding universe
In 2020, during the height of the COVID-19 pandemic, it was clear that some infected people became severely ill, while others were barely infected by inhalation. A massive consortium of scientists, led by pediatrician and immunologist Jean-Laurent Casanova at Rockefeller University in New York City, has discovered that about 10% of people with severe cases of COVID-19 have autoantibodies — rogue proteins that turn against the person’s body. These autoantibodies attacked the signaling molecules that help mobilize the immune response, weakening immune defenses5.
Casanova and his colleagues have since found the same autoantibodies in a subset of people who became severely ill with seasonal influenza, West Nile, and several other diseases, as well as in those with rare adverse reactions to live vaccines, such as the yellow fever vaccine.

How the first brush with the Corona virus distorts your immunity
It is not known exactly why and how autoantibodies develop. Some scientists, including Casanova, suspect that it may be the result of inherited or acquired mutations. He and others have identified some mutations that can lead to these autoantibodies, such as deficiencies in various interferon-related genes. It remains to be seen whether these mutations could be responsible for the majority of severe cases of these diseases.
Researchers are still working on the complex ways in which genes contribute to infection outcomes. Having a mutation does not always make a person vulnerable: IEIs can behave unpredictably. Many people carry mutations associated with immunodeficiency without ever experiencing their effects — a phenomenon known as “incomplete penetrance.” Although most severe IEI symptoms become evident in childhood, some may remain dormant for decades. In unpublished work, Metts and her team identified a person who had a mutation associated with an inflammatory disease, but whose symptoms only developed after infection with SARS-CoV-2.
Scientists are still working to determine the factors that affect the severity of IEIs. In a 2025 study, Dusan Bojonovic, a pediatric immunologist at Columbia University in New York City, and colleagues discovered that in about 4% of IEI cases, the disease-causing variant could be expressed differently in different cells.6. The team also found evidence that this process may be regulated through epigenetic mechanisms, which are influenced by environmental factors – suggesting that not only may the same IEIs appear differently in different people, but the effects of these mutations can change over the course of a person’s life. Bojonovic’s team is currently looking for factors, such as inflammation or certain infections, that might control the expression of this variant allele.
